In our previous posts, we discussed various factors influencing dental implant failure. In this post, we will specifically focus on patient-related factors that can affect dental implant failure.
(1) Poor Bone Quality and Quantity
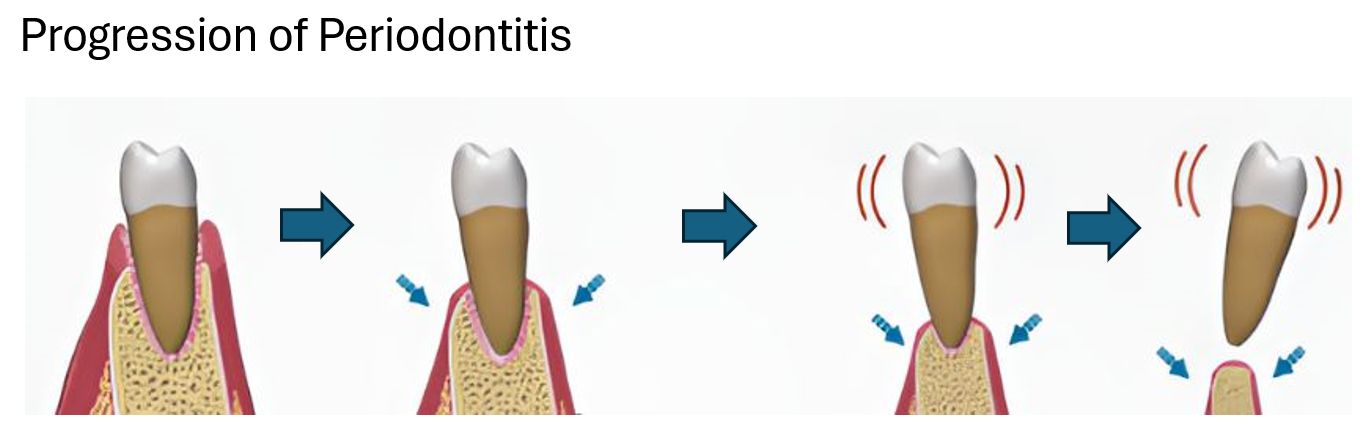
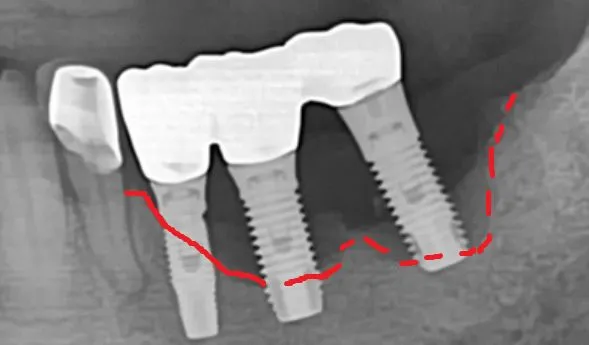
Many individuals lose their teeth due to periodontitis (gum disease). While some seek gum treatment to save their natural teeth upon their dentist’s recommendation, others do not. If not cared properly, the bone surrounding the remaining teeth can become progressively diminished in both quantity and quality. When patients present with severely mobile teeth due to advanced bone loss, they often lack sufficient bone to support dental implants. In such cases, the prognosis for dental implant success can be somewhat compromised.
(2) Systemic Disease: Diabetes

Diabetes is a significant systemic health issue that can impact the success of dental implant treatment. Poorly controlled diabetes can complicate implant procedures and elevate the risk of failure due to impaired healing, increased susceptibility to infection, and compromised bone metabolism. Then, what exactly constitutes poorly controlled diabetes?
Glycemic Control is Paramount: The most critical factor is the patient’s blood glucose control, typically measured by HbA1c levels. The consensus, supported by the 2018 ADA/EASD (American Diabetes Association/ European Association for the Study of Diabetes ) report and the 2020 Wagner review, suggests that patients with HbA1c levels below 7.0% or 7.5% generally have similar implant success rates to non-diabetic individuals. Higher HbA1c levels are associated with increased risks.
Consequently, for diabetic patients, maintaining an HbA1c level below 7.5%, with a target of under 7.0%, is strongly recommended to optimize dental implant success. Post-operatively, the following may be advised:
- Prophylactic antibiotics
- Extended post-surgical antibiotic regimen
- Chlorhexidine mouth rinse
- Bio-active material coated implants
(3) Systemic Disease: Osteoporosis

Osteoporosis, characterized by reduced bone density, can raise concerns regarding dental implant success due to potentially impaired bone healing.
However, a diagnosis of osteoporosis does not automatically disqualify someone from receiving dental implants. Careful evaluation and treatment planning are essential. Research on the direct impact of osteoporosis on implant failure rates has yielded mixed results. While some meta-analyses suggest no significant difference in implant survival rates between patients with and without osteoporosis, other studies indicate a higher risk of marginal bone loss around implants in osteoporotic individuals, which could affect long-term stability. It is particularly important to inform your dentist if you are taking Bisphosphonates or RANKL inhibitors, as these medications have been associated with a rare but serious condition called osteonecrosis of the jaw.
(4) Smoking
Smoking is a major factor that negatively affects dental implant outcomes. It impairs blood flow to the gums and jawbone, increases the risk of infection, and delays wound healing. Consequently, studies have shown that smokers experience dental implant failure rates 2 to 3 times higher than non-smokers.
(5) Poor Oral Hygiene
Maintaining excellent oral hygiene is paramount for the longevity of dental implants. This includes diligent daily brushing and flossing, as well as regular professional dental check-ups and cleanings.
(6) Grinding and Clenching (Bruxism)
Bruxism, the habit of grinding or clenching teeth, exerts excessive and repetitive forces on dental implants. This can impede osseointegration, the critical process of implant fusion with the jawbone, potentially leading to early implant failure. Unlike natural teeth, dental implants lack the cushioning effect of the periodontal ligament (indicated by the green arrow below), which absorbs stress. To use an analogy, if natural teeth are like sneakers designed to absorb impact, implants are more like dress shoes. Running in dress shoes would strain your ankle, unlike running in sneakers.

Furthermore, dental implants lack sensory nerves, so patients may not feel the damaging overload until serious issues like screw loosening (leading to crown loosening), implant fracture, damage to the restoration, or bone loss around the implants manifest. Consequently, we strongly advise the use of a nightguard to protect both the implants and the opposing natural teeth.

Boston Finesse Dentistry & Implant Center
183 Essex St, Boston MA 02111 | 617-286-6515 (Call/Text) | SLee@BostonImplant.com
References:
Buse JB, Wexler DJ, Tsapas A, Rossing P, Mingrone G, Mathieu C, D’Alessio DA, Davies MJ. 2019 update to: Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2020 Feb;63(2):221-228. doi: 10.1007/s00125-019-05039-w. Erratum in: Diabetologia. 2020 Aug;63(8):1667. doi: 10.1007/s00125-020-05151-2. PMID: 31853556.
Wagner J, Spille JH, Wiltfang J, Naujokat H. Systematic review on diabetes mellitus and dental implants: an update. Int J Implant Dent. 2022 Jan 3;8(1):1. doi: 10.1186/s40729-021-00399-8. PMID: 34978649; PMCID: PMC8724342.