Dental implants have become a popular solution for replacing missing teeth. However, like any medical procedure, they can sometimes fail. In this post, we’ll discuss key factors that can affect dental implant failure.
(1) Misaligned Implants
Unfortunately, some dental implants are placed based on guesswork, resulting in suboptimal location, angle, and depth.
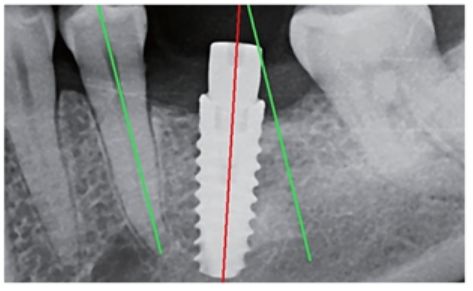

In my experience, precise implant placement is paramount for a successful outcome. If an implant is positioned at an incorrect angle, the off-center pressure can compromise its stability. This can lead to short-term issues like crown or screw loosening and, ultimately, long-term implant failure. This is why I always use surgical guide even the simplest implant.
(2) Failure of Osseointegration
Osseointegration is the process by which a dental implant, typically made of biocompatible materials like titanium, securely fuses with the surrounding jawbone. This fusion provides a stable and durable foundation for the replacement tooth. Sometimes, this crucial process fails due to several reasons:

- Inadequate Primary Stability: If the implant isn’t placed firmly enough in the bone initially, even slight micromovement can disrupt the delicate healing process and prevent proper bone growth around the implant.
- Poor Dental Implant Quality: The quality of dental implants can vary significantly between brands. Some lower-quality implants may exhibit lower osseointegration success rates. (Check out our post about ‘Best dental implant brand’ for more information.)
- Overheating of Bone: Excessive heat generated during the drilling process (due to dull drills, insufficient irrigation, or excessive speed) can damage bone cells and hinder proper healing and integration.
- Surgical Trauma: Excessive trauma to the surrounding bone and soft tissues during the surgical procedure can impede healing. This includes both physical trauma and thermal damage (overheating).
(3) Poor Crown Design (Emergence Profile)
The emergence profile is the contour of the restoration where it emerges from the implant and surrounding soft tissues. It’s influenced by factors such as implant position and the health of the adjacent gums. A well-designed emergence profile should be biologically acceptable (promoting healthy tissues), easily cleanable by the patient, and aesthetically pleasing.

Crown B illustrates a poor emergence profile. Its bulk near the bone area can lead to thin connective tissue. Additionally, the absence of platform switching (a design feature that helps reduce initial bone loss around the top of the implant) can exacerbate bone loss. Over time, Crown B is likely to contribute to bone loss around the implant (as indicated by the change in the green line).
Often, patients with poorly designed crowns don’t recognize the issue initially. It might not be painful, just a mild discomfort. However, this seemingly minor problem can lead to severe complications later on. I always prioritize the use of custom abutment to create ideal emergence profiles, ensuring both the longevity and aesthetics of the implant restoration. (Refer to my post about the ‘Custom abutment‘ further details.)
(4) Implant Fracture

While dental implants are strong, they can sometimes fracture, or their internal components (like abutment screws) can strip. Most dental implants placed today are internal connection implants, which are generally reliable when the implant diameter is sufficient and the placement is correct. However, their inherent design can result in a thinner top collar area, making them potentially susceptible to fracture or stripping. To mitigate this risk, I often prefer tissue-level implants, which typically have a thicker top collar area. (Refer to my post about the ‘Best dental implant type‘ for further details.)
(5) Complications in Guided Bone Regeneration (GBR)

Many dental implant patients require bone grafting to achieve sufficient bone volume, ranging from simple grafts to complex sinus lifts. These procedures can sometimes be compromised, leading to wound dehiscence (opening) or infection. Minimizing these complications requires reliable surgical skills, the selection of optimal grafting materials, and meticulous contamination management.
In our upcoming post, we’ll be exploring the patient factors that can impact dental implant failure. Don’t miss it!
Why Focusing on Failure Rates Matters
Some implant dentists boast high success rates, often in the range of 96-98%. While these numbers seem impressive, they also imply a failure rate of 2-4%. Let’s put this into perspective: with a 97% success rate, the failure rate is 3%, meaning approximately 3 out of every 100 implants, or 1 out of every 33 implants, could fail. This isn’t an insignificant number.
While many implant dentists emphasize their success rates, I believe it’s equally, if not more, important to focus on minimizing the failure rate. My personal failure rate is lower than 0.5%, meaning I rarely encounter implant failures in a year. Dental implants can fail, but by adhering to best practices in every aspect of the treatment, we can significantly reduce the likelihood of these failures.
Boston Finesse Dentistry & Implant Center
183 Essex St, Boston MA 02111 617-286-6515 (Call/Text) SLee@BostonImplant.com